Introduction
Embark on a journey into sustained success within the complex realm of Revenue Cycle Management (RCM). This case study unveils the strategies behind consistently maintaining Accounts Receivable (AR) below 5% beyond the critical 90-day mark. Discover actionable insights tailored for professionals navigating the intricacies of RCM in the U.S. healthcare landscape. Join us as we explore the keys to sustaining a lean AR balance, ensuring enduring financial excellence in healthcare operations
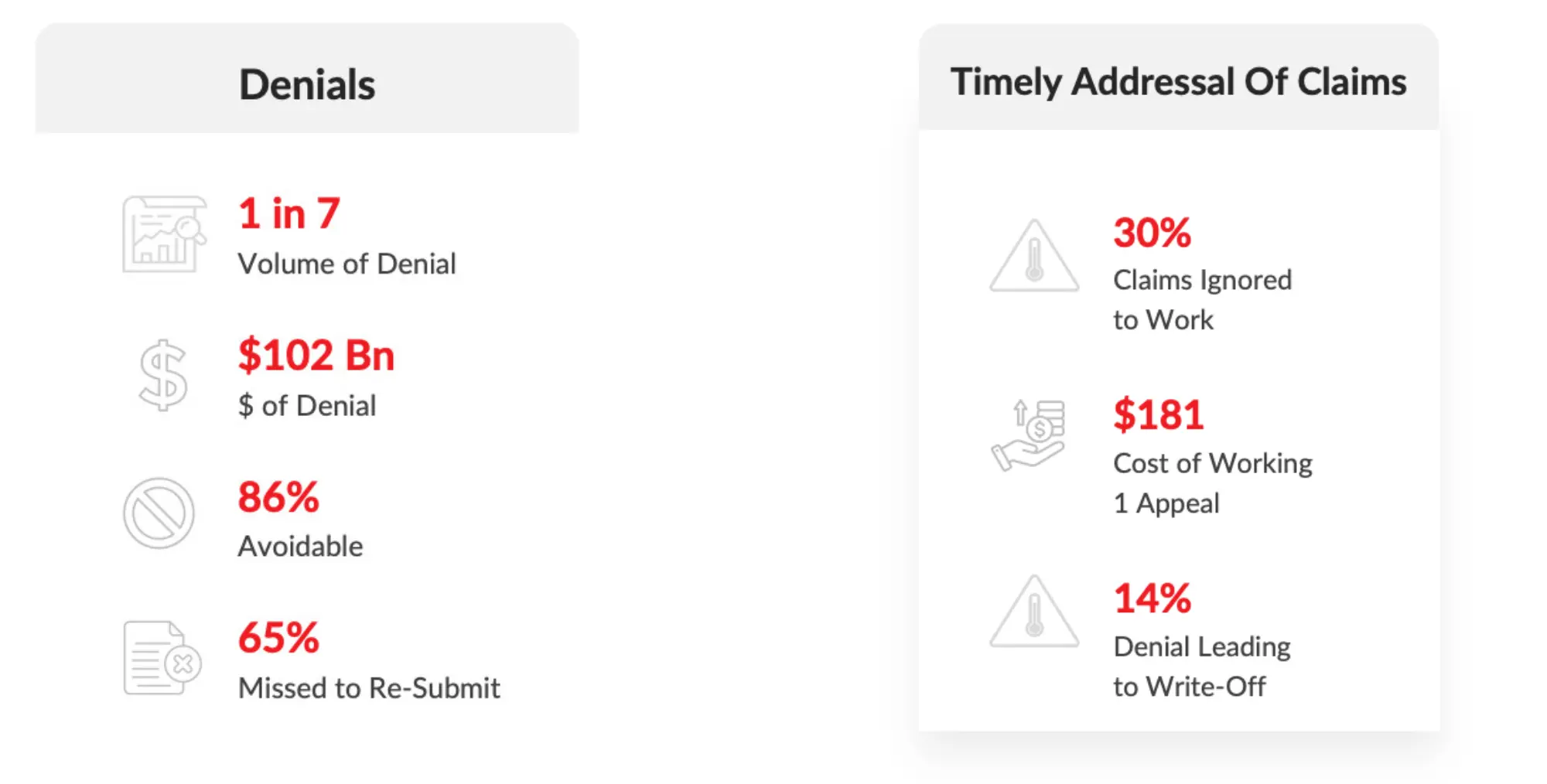
Industry Challenges - Insights
Problem statement
- Inefficient Eligibility & Benefits Verification.
- Higher Medical Necessity denials.
1. Denials Untouched, high denials are:
2. In-Appropriate Payment Posting.
3. Claims not followed up on time.
4. Appeals have not worked and have not followed up.
5. Resolution of claims <90 days was lagging.
Root Cause
- A defined process for Eligibility and benefits Verification was missing
- Due to a shortage of staff, the actions were not taken promptly
- The eligibility process was all manual which further delayed the process
- The coding process was not streamlined
- Leveraging required tools and systems to determine efficient and compliant - reimbursement coding was not in place
- Misalignment between the services provided and the payer's criteria for necessity
- The payment poster's knowledge and lack of understanding of offsets and recoupments led to an unreconciled balance
- Lack of Prioritization: A perennial challenge in the industry, prioritizing a high volume of claims requires comprehensive data analytics and data intelligence tools which was missing
- Again, shortage of staff is another critical issue
- Overload of Work - A shortage of staff will lead to an Overload of work and impact the efficiency of productivity and accuracy
- The consequence of timely addressal of denials, and following up on claims due to reasons highlighted above leads to Appeals not working timely
- Effective claim resolutions require an organization to pull off multiple levers together concurrently
- Claims less than 90 days were not worked effectively
- Reasons, every claim requires follow-up every 30 days
- Early insights on payment denials missed has a multitude effects on current, future, and past claims.
- The multitude effect become multifold making the AR more complex and hard to collect
- Inefficient Work-Flow system.
Our objective was to comprehensively analyze the challenges posed by extended AR cycles and, in turn, equip decision-makers with actionable strategies to navigate this impending threat effectively.
1. Inefficient Eligibility & Benefits Verification
2. Higher Medical Necessity Denials
1. In-Appropriate Payment Posting
2. Claims not followed up on time
1. Appeals have not worked and have not followed up
2. Resolution of claims < 90 days was lagging
Solutions for Root Cause - Coding Services
- Coding Process
- Documentation Improvement
- Revamped coding guideline documentation upon careful review of all denials
- Coding documentation feedback by deployingSenior Coding professionals
- Tracked all denials post-go-live to reduce coding denials
Root Cause
Solutions
Solutions for Root Cause - Cash Posting Services
- In-appropriatePayment posting dueto offsets andRecoupments
- Unreconciled Claim balances
- Complete EOB review of all open claims with high priority on high $ value claims
- Reasons for recoupments, offsets tracked and streamlined by deploying Senior Payment posters
- Leveraged in-house Cash Reconciliation tools to speedy completion,
Root Cause
Solutions
Solutions for Root Cause - Technology (Prior Auth Smart)
- Eligibility & Benefits Process in-effective
- No effective work-flow
- Completed all payment posting issues
- Cleaned up by moving balance appropriately - to Patient & Insurance
- Deployed our internally developed Technology solutions
- Benefits & Eligibility Process Streamlined
Root Cause
Solutions
Solutions for Root Cause - Technology (RevShield A.I.)
- Claims not followed-up Timely
- Prioritization of claims
- Comprehensive Data Analytics & Intelligence tool.
- Extensive technology implementation to roll up to RevShield A.I.
- Implemented Machine Learning Algorithms to learn denial patterns.
- Data Intelligence modules started to provide deeper insights on Aging, Denials, Trends & patterns including Resolution Rate - # of touch resolutions
Root Cause
Solutions
Discover the Results: Dive deeper into our case study to explore the outcomes and results of our strategies that enabled our clients to maintain AR > 90 days at LESS THAN 5%. Click here to read more!
Read More


